Health and well-being in the EU: Investing where it matters
A data-driven look at prevention spending, disease burden and access to care across the EU
Good health is a personal goal but also the foundation of a resilient society. Across the EU, health systems do more than treat illness – they aim to help people live longer, better lives. In recent years, this goal has gained momentum, with initiatives like Europe’s beating cancer plan, the European health union and the European health data space pushing for stronger prevention, earlier diagnoses and better access to care across Member States.
But as Europe’s healthcare systems face new pressures, it is worth asking: are we putting our resources where they matter the most? How is investment distributed between preventive and curative care? What are the leading causes of premature deaths in the EU, and to what extent might some of them be prevented through timely care or healthier lifestyles? Finally, why do some people still struggle to access care?
Using open data, this story explores these questions, offering insights into where better alignment between spending, needs and outcomes could lead to lasting improvements.
How are healthcare funds used?
Healthcare systems do not just treat illness – they also play a key role in keeping people healthy in the first place. Preventive care, including vaccinations, screenings and health education, can reduce the burden of disease, improve quality of life and help avoid costly treatments. Yet, in systems under pressure from ageing populations, chronic diseases and rising costs, prevention often competes with more immediate needs like hospital and emergency care.
Open data on healthcare spending sheds light on how countries distribute public health budgets across a mix of services that include curative treatment, rehabilitation, long-term care, prevention and other areas.
As shown in Figure 1, the share of spending on prevention remained stable throughout much of the last decade, with an increase after 2020 due to COVID-19 response measures.
In 2022, preventive services accounted for 5.5 % of the EU’s total healthcare expenditure. The largest share went to curative and rehabilitative care (51.9 %), followed by medical goods like pharmaceuticals (17.8 %) and long-term care (16.2 %). While this general pattern holds across all Member States, spending on prevention ranges from 8 % in Germany to 1–2 % in countries like Poland, Slovakia (2 %) and Malta (1 %).
These figures do not in themselves indicate what the ‘right’ level of prevention spending should be, as that depends on many factors, including the effectiveness of interventions, national priorities and population needs. Still, understanding how resources are allocated offers a starting point for further exploration. Looking at the leading causes of premature death across the EU may help identify where preventive care might have the biggest impact.
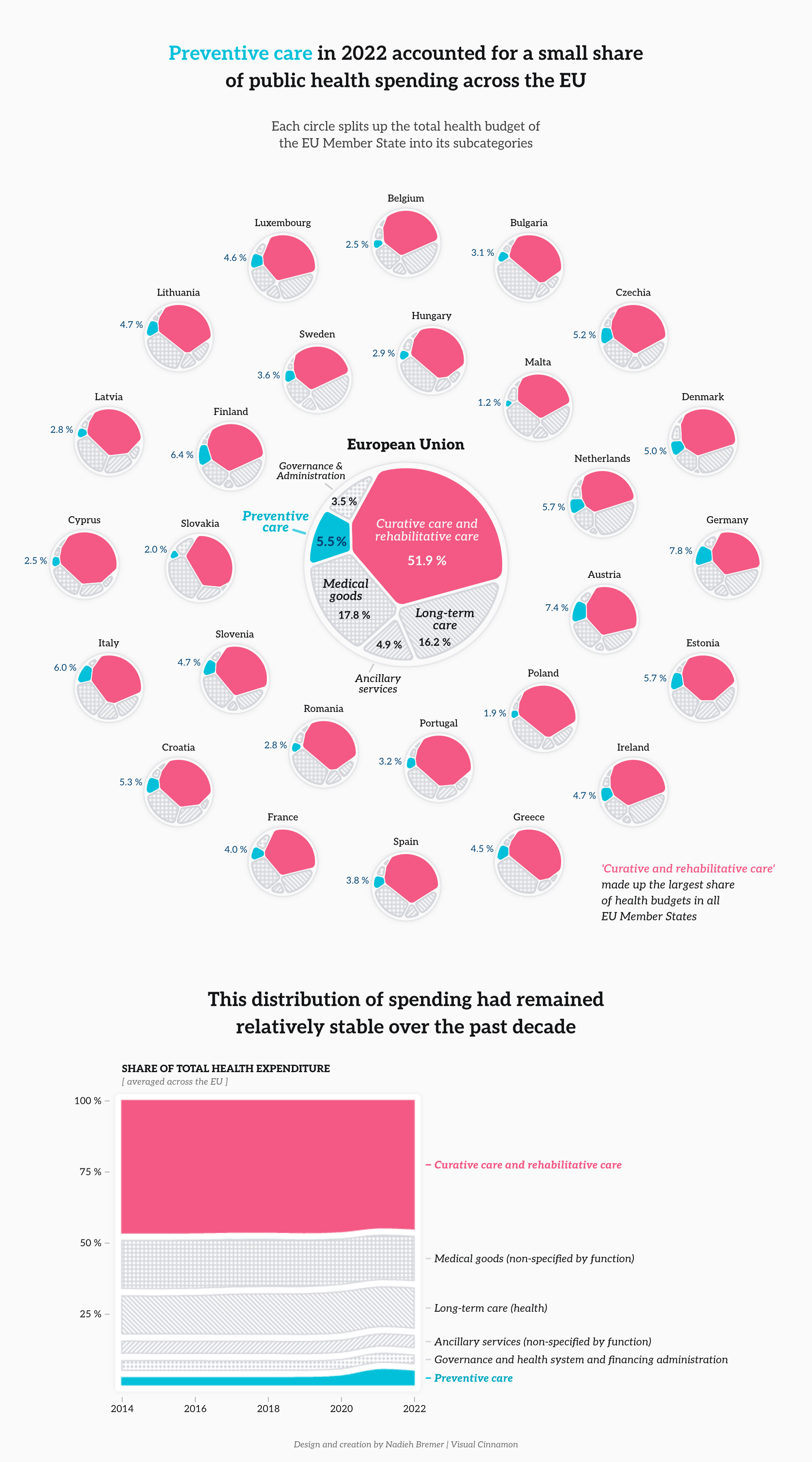
Figure 1: EU spending on overall healthcare and preventive care (2022)
Source: Eurostat, data.europa.eu.
What are the leading causes of early death in the EU?
In 2022, 1.6 million people in the EU died before reaching the age of 75. Understanding the causes behind these early deaths helps identify where public health efforts – such as prevention and timely treatment – could make the greatest difference.
Figure 2 shows the leading causes of death across the EU in 2022, grouped into three categories: preventable, treatable or unavoidable. Preventable and treatable causes together make up the category of avoidable deaths, referring to those that could have been averted either through effective public health measures or timely healthcare interventions.
Only one third (33 %) of deaths before age 75 resulted from causes considered unavoidable. In contrast, 44 % were linked to preventable causes – often associated with modifiable risk factors such as smoking, alcohol use or environmental exposure. Another 23 % stemmed from causes that are considered treatable, meaning they could have potentially been avoided through timely and effective healthcare.
The leading avoidable cause of death, accounting for 9.4 % of all deaths below age 75, was ischaemic heart disease – a condition where narrowed arteries reduce blood flow to the heart, often leading to heart attacks. Because this condition is considered both preventable and treatable, Eurostat allocates it equally to both categories. Other leading causes include lung cancer (8.2 %, mostly preventable), COVID-19 (4.3 %) and colorectal cancer (3.5 %).
The high share of deaths due to avoidable causes underscores the importance of strengthening public health strategies. Strengthening public health programmes and early intervention can have a measurable impact on the EU’s overall health outcomes.
Yet, offering services is only part of the solution. To make healthcare systems more effective and inclusive, we must also understand how people interact with them – and why, in some cases, they do not. In the next section, we explore the barriers that prevent individuals from accessing the care they need.
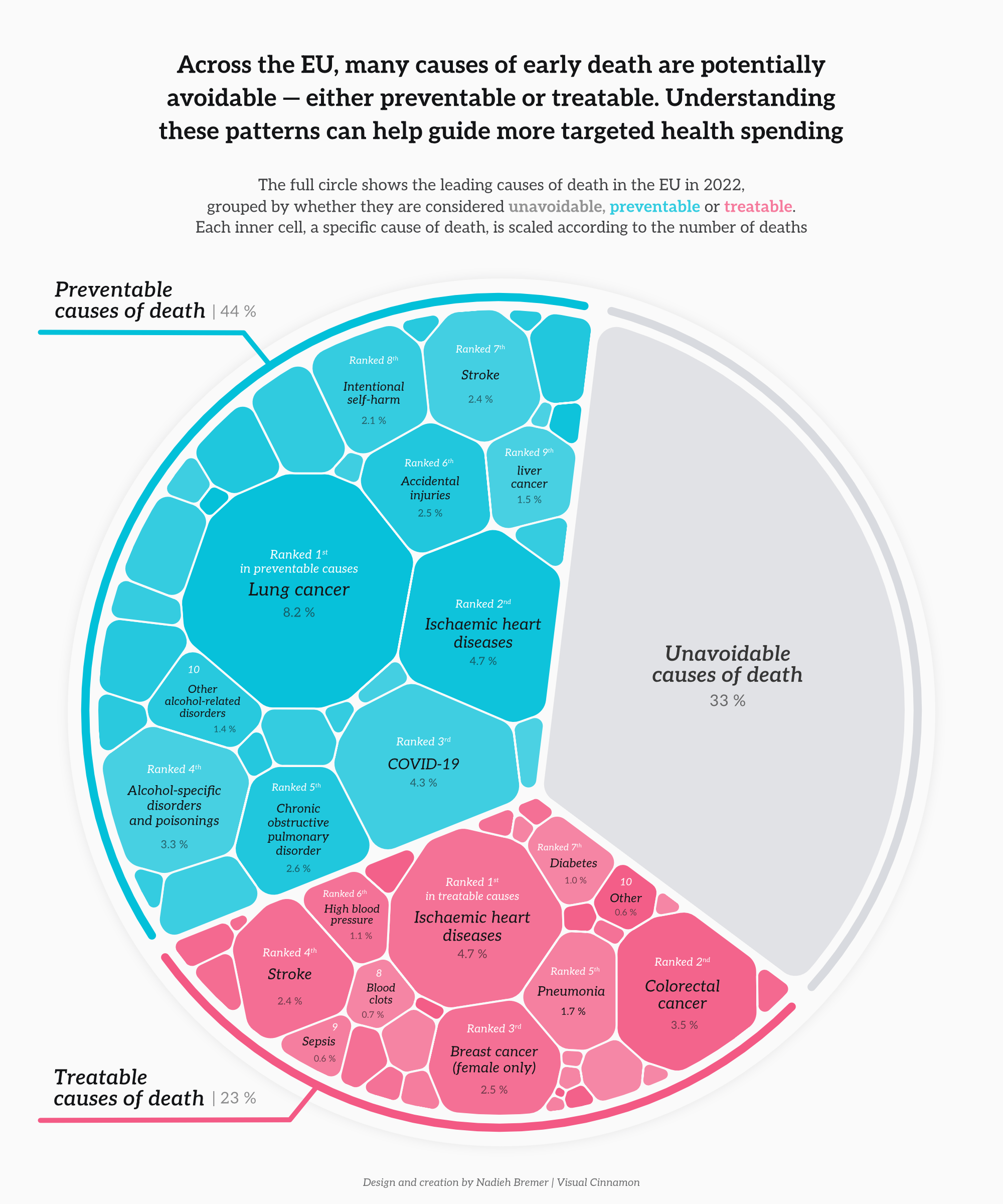
Figure 2: Preventable, treatable and unavoidable causes of death in the EU for people aged under 75
Source: Eurostat, data.europa.eu.
Why do people not obtain medical examinations/treatment?
Even when healthcare systems are in place and effective treatments exist, many people across the EU still face unmet health needs. Whether due to cost, distance, long waiting times or personal hesitation, these missed opportunities can allow manageable health conditions to worsen – undermining both individual well-being and broader public health goals.
Open data from 2024 on self-reported unmet needs for medical care provides insight into the real-life barriers people encounter. These barriers are not just about the availability of services, but also about the accessibility and affordability of services and the trust people place in the system.
At the EU level, 3.8 % of people aged 16 or over reported that they needed a medical examination or treatment in the previous 12 months but did not receive it. The most commonly cited reasons were long waiting times (1.4 percentage points, or slightly more than one third of all cases of unmet medical needs), high costs (1 percentage point, or slightly more than 25 % of all cases of unmet medical needs) or hoping the issue would resolve on its own (0.4 percentage point, or slightly over 10 % of all cases of unmet medical needs). These factors vary widely across age groups, income levels and – as shown in Figure 3 – countries.
Understanding these barriers is essential for building more inclusive, patient-centred healthcare systems. Identifying not just who is left out, but why, allows policymakers at all levels to develop targeted solutions that improve access, reduce inequality and ensure timely care for all.
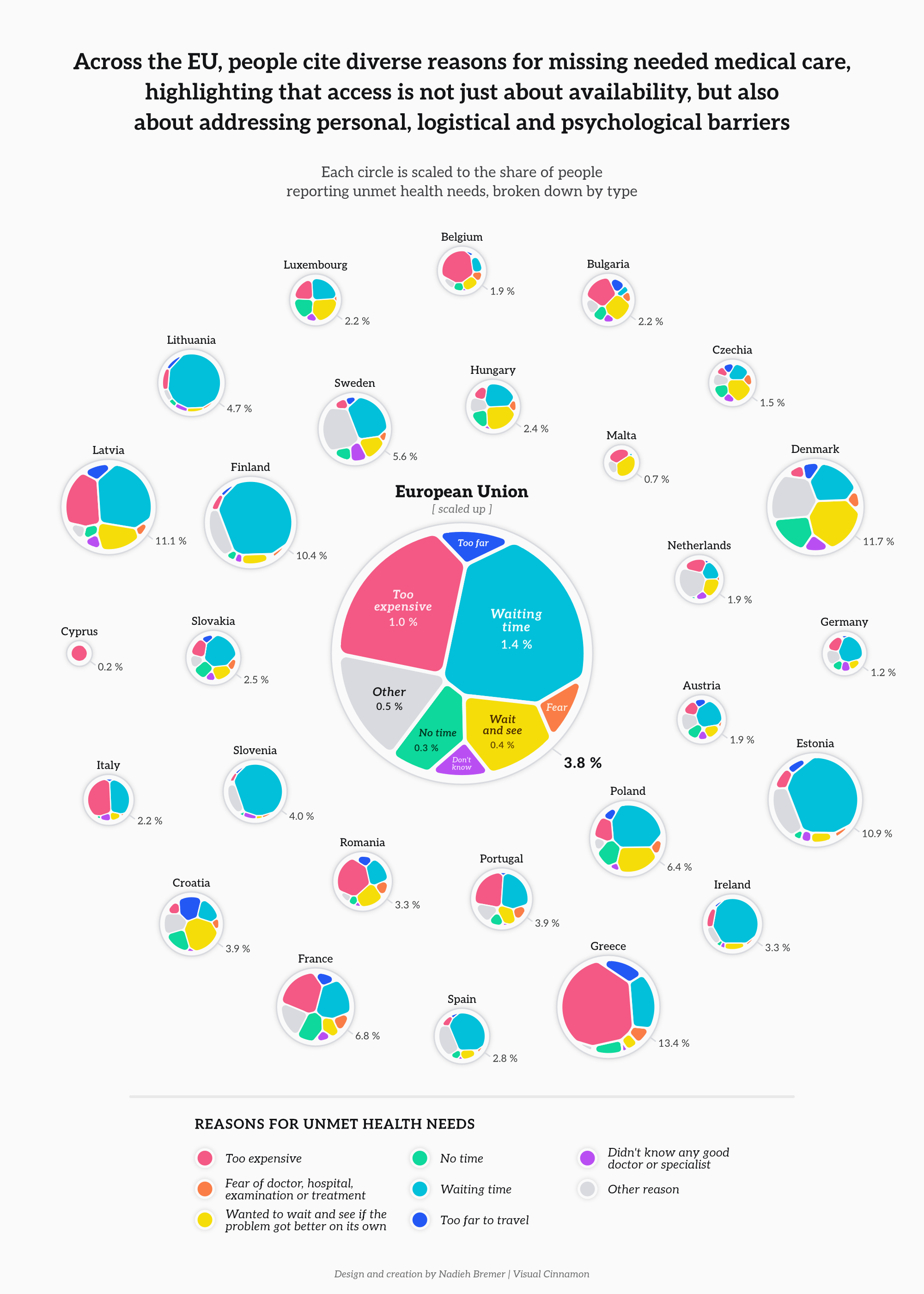
Figure 3: Reasons for unmet health needs across the EU for people aged 16 years or over (2024)
Source: Eurostat, data.europa.eu
Conclusion
Health outcomes across Europe are shaped not only by the availability of care, but also by how healthcare systems allocate resources and respond to real-world barriers. This data story examined three dimensions of public health in the EU: the distribution of healthcare spending, the leading causes of avoidable mortality and the factors that contribute to unmet medical needs.
The data highlights possible discrepancies. Preventive care continues to account for a small share of healthcare budgets, while a large proportion of deaths under 75 result from causes that could be prevented or treated. In parallel, barriers such as cost, distance and waiting times persist across countries, affecting access to timely care – especially for those in vulnerable situations.
These findings offer insight into how health systems function in practice and where mismatches may exist between investment, outcomes and access. Open data enables such patterns to be identified and compared – supporting more informed decision-making at both the national and EU levels.
